
Reversing Insulin Resistance: What You Need To Know
Daniel Murphy // Dietitian, Cork // April 24
Are you struggling with insulin resistance and its impact on your health? If so, you’re not alone. Insulin resistance is a condition that affects millions of people worldwide and can be linked with health conditions like obesity, diabetes, and heart disease. But the good news is that it does not have to be permanent. Personally, I prefer to use the terminology “improve” over “reverse” as it’s not a switch. It’s a gradual improvement overtime. However it’s important to differentiate between Type 2 Diabetes and insulin resistance. Current research suggests Type 2 Diabetes itself is not reversible, but if only looking to tackle or improve insulin resistance, you can definitely can achieve this.
In this comprehensive guide, we’ll walk you through everything you need to know about reversing insulin resistance. From understanding the causes and symptoms to implementing effective strategies for improvement, we’ve got you covered. We’ll dive into the science behind insulin resistance, explore the role of diet and exercise, and even discuss alternative methods that may support your journey to better health.
Whether you’re new to the concept of insulin resistance or you’ve been struggling to make progress, this guide is designed to provide you with the information and tools you need to take control of your health. Get ready to transform your life and reverse insulin resistance for good.

Table of Contents
Understanding Insulin Resistance
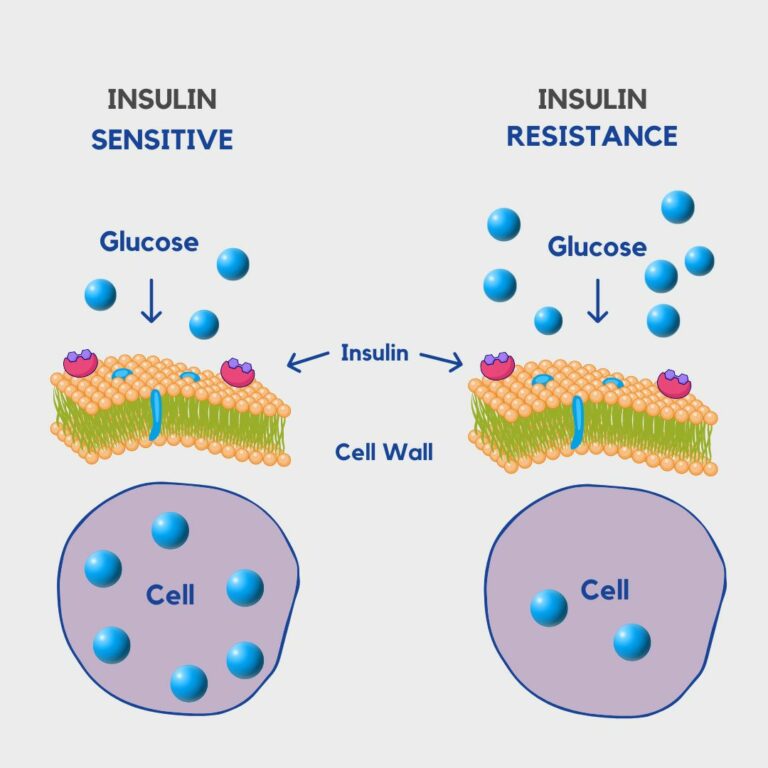
Insulin resistance is a condition in which the body’s cells become less responsive to the hormone insulin. Insulin is produced by the pancreas and plays a crucial role in regulating blood sugar levels. When cells become resistant to insulin, the pancreas produces more insulin to compensate, leading to elevated levels of insulin in the blood. Check out the image below as an example of how this process works.
Causes and Risk Factors of Insulin Resistance
Insulin resistance can be caused by a combination of genetic and lifestyle factors. Some of the common risk factors include obesity, sedentary lifestyle, poor diet, and certain medical conditions like polycystic ovary syndrome (PCOS). Genetics also play a role, as some individuals may be more predisposed to developing insulin resistance.
To improve symptoms of insulin resistance, aim to focus on:
- A balanced diet
- Regular exercise both cardio and resistance training if possible
- Reducing BMI to a healthy range. Check out our BMI calculator to find out yours.
Signs and Symptoms of Insulin Resistance
Insulin resistance often develops gradually, and its symptoms may be subtle at first. Some common signs of insulin resistance include:
- Difficulty losing weight, especially around the abdomen,
- Increased hunger and cravings,
- Fatigue
If left untreated, insulin resistance can progress to pre-diabetes and eventually type 2 diabetes. The diagram below shows that energy (glucose) from food finding it difficult to enter the cell to provide energy. This is mainly why fatigue can be a big issue with the condition.
The Impact of Insulin Resistance on Health
Insulin resistance has far-reaching effects on overall health. It increases the risk of developing type 2 diabetes, which can lead to serious complications such as heart disease, kidney damage, and nerve damage. Insulin resistance is also associated with an increased risk of obesity, high blood pressure, and abnormal cholesterol levels. Addressing insulin resistance is crucial for preventing these long-term health complications.
Testing and Diagnosing Insulin Resistance
If you suspect you may have insulin resistance, it’s important to consult with a healthcare professional for proper diagnosis and testing. Several tests can be used to assess insulin resistance, including:
These tests help determine the severity of insulin resistance and are often common biomarkers for the diagnosis of Pre-Diabetes and Type 2 Diabetes.
Treating Insulin Resistance through Lifestyle Changes
The cornerstone of reducing the effects of insulin resistance lies in making significant lifestyle changes. These changes primarily focus on improving diet, increasing physical activity, and maintaining a healthy weight. By implementing these changes, you can improve insulin sensitivity and restore your body’s ability to regulate blood sugar effectively.
The Role of Diet in Reversing Insulin Resistance
A healthy diet is crucial for reversing insulin resistance. The key is to focus on whole foods that are low in added sugars and refined carbohydrates. Carbohydrates aren’t always the enemy, it’s the type and quantity of carbohydrates that play the biggest role in this condition. We want to reduce and moderate refined carbohydrates such as sweets, chocolate and biscuits. However, we don’t want to totally exclude them.
Instead, opt for nutrient-dense foods like fruits, vegetables, lean proteins, and healthy fats. Wholegrain carbohydrates can also be very beneficial. Look to pair these with a protein and a fat source. For example, having brown pasta with salmon is a great way to slow down the insulin response to a carb. Always look to pair food groups to aid in this process.
Additionally, controlling portion sizes and eating at regular intervals can help stabilise blood sugar levels and improve insulin sensitivity.
Struggling with Weight Loss?
Physical Activity and Exercise for Insulin Resistance
Regular physical activity and exercise play a vital role in reversing insulin resistance. Engaging in both aerobic exercises and strength training can help improve insulin sensitivity and promote weight loss. A mix of both strength training and cardio is ideal as insulin sensitivity increases in a response to exercise. If you’re not into exercise, try a brisk walk, as any movement will be a huge benefit.
Why is this you may ask? After any form of exercise our muscles require extra energy for recovery so soak up a lot more energy from food, specifically carbohydrates at this time.
Aim for at least 150 minutes of moderate-intensity aerobic activity per week, along with two or more days of strength training exercises.
Medications and Supplements for Managing Insulin Resistance
In some cases, lifestyle changes alone may not be sufficient to improve insulin resistance. This is mainly in extreme cases. Medications may be needed but mainly only in conditions like Type 2 Diabetes. These medications may include metformin, which is one of the most commonly used. Additionally, certain supplements like inositol are used in PCOS a lot to promote insulin sensitivity. Remember, supplements will do 5% of the work. Much of the answers lie in nutrition and exercise.

Long-term Strategies for Preventing Insulin
Resistance Recurrence
Reversing insulin resistance is just the first step towards optimal health. To prevent its recurrence, it’s important to maintain healthy lifestyle habits in the long term. This includes continuing to follow a balanced diet, engaging in regular physical activity, managing stress levels, and getting adequate sleep.
We at Apex Nutrition really look to support this long term change through behaviour change and nutrition programs. If insulin resistance is something you’d like to learn more about, then feel free to reach out here.
Reversing insulin resistance is a journey that requires dedication and commitment. By understanding the causes, symptoms, and impact of insulin resistance, you can take the necessary steps to improve your health. Through lifestyle changes, including a healthy diet, regular exercise, and, if necessary, medication or supplements, you can restore your body’s ability to regulate blood sugar and prevent long-term health complications. Remember, you have the power to take control of your health and reverse insulin resistance for good. Start your journey today and embrace a healthier, insulin-sensitive future.
Frequently Asked Questions
Insulin resistance is a condition where the body’s cells become less responsive to insulin, a hormone responsible for regulating blood sugar levels. As a result, blood sugar levels may rise, leading to potential health complications.
Insulin resistance can develop due to various factors, including genetics, excess body weight, sedentary lifestyle, unhealthy diet high in refined carbohydrates and sugars, chronic stress, and lack of physical activity.
Common symptoms of insulin resistance include fatigue, increased hunger, difficulty losing weight, frequent urination, increased thirst, and dark patches of skin, especially around the neck or armpits (acanthosis nigricans). However, some individuals may not exhibit any noticeable symptoms.
Insulin resistance is often diagnosed through blood tests that measure fasting blood glucose levels, insulin levels, and sometimes a glucose tolerance test. Additionally, healthcare providers may assess other risk factors such as waist circumference and family history.
Yes, insulin resistance can often be reversed or improved with lifestyle changes. These may include adopting a healthy diet rich in whole foods, increasing physical activity, managing stress levels, getting adequate sleep, and, in some cases, medications prescribed by a healthcare professional.
Foods to avoid or limit if you have insulin resistance include sugary beverages, refined carbohydrates (such as white bread, pastries, and sugary snacks), processed foods high in unhealthy fats, and excessive intake of alcohol.
If left untreated, insulin resistance can lead to serious health complications such as type 2 diabetes, cardiovascular disease, high blood pressure, stroke, kidney disease, and certain cancers. However, early intervention and lifestyle changes can help prevent or delay these complications.
Yes, regular physical activity, including both aerobic exercises (such as walking, jogging, or cycling) and resistance training, can improve insulin sensitivity, lower blood sugar levels, and aid in weight management, thereby helping to manage or reverse insulin resistance.
While some supplements, such as chromium, magnesium, and alpha-lipoic acid, have been studied for their potential benefits in improving insulin sensitivity, it’s important to consult with a healthcare provider before taking any supplements. Inositol is often used to increase inulin sensitivity in PCOS. However, diet and exercise will be the most effective route.
The timeline for seeing improvements in insulin resistance can vary depending on individual factors such as starting weight, genetics, and the extent of lifestyle changes made. However, many people may begin to see improvements in blood sugar levels and insulin sensitivity within a few weeks to months of adopting healthier habits. Regular monitoring and consistency in lifestyle changes are key for long-term success.
